Adults living with CF can face many comorbidities, including CFRD, reflux and bone disease, all of which can be impacted and/or managed with diet.
Cystic Fibrosis Related Diabetes
Cystic Fibrosis Related Diabetes (CFRD) is a type of diabetes unique to people with CF. It is different to other types of diabetes and the symptoms may vary from person to person. It is caused by damage to the pancreas over a period of time. It may be triggered by an exacerbation and treatment of an infection and/or be a gradual onset; it is not related to diet. Individuals with CF should be tested annually for the development of CFRD and following diagnosis, should have a six-monthly dietary review or more often if required.
One of the pancreas’ main jobs is to make and secrete a hormone called insulin. Insulin helps glucose from food get out of the blood and into the cells in our bodies to be used for energy. Insulin is considered the ‘key’ that ‘unlocks’ the cells. If glucose cannot get into our cells, they cannot work properly.
- Hyperglycaemia: A reduced amount of insulin production results in high blood glucose levels (BGLs), known as hyperglycaemia. In a person with CF, symptoms may include a lack of energy, a decrease in lung function, weight loss, increased hunger, excessive thirst and increased urine output.
- Hypoglycaemia: Or a ‘hypo’ is when the opposite occurs and BGLs drop too low. Signs of a hypo can include hunger and feeling shaky followed by sweating and possibly fainting.
Insulin and other diabetes medications are used to help the body use glucose effectively and keep BGLs at near-normal levels. This will help to maintain your weight and ensure good health. Everyone is different and so individualised dietary advice from a specialist diabetes team experienced in the management of CFRD is essential.
Food
The nutritional management of CFRD is different to that of type 1 or type 2 diabetes. In general, if you are pancreatic insufficient and have CFRD you will still need to eat a high calorie, unrestricted diet to maintain your weight. Although optimising BGLs is important in CFRD, this should not be at the expense of eating enough calories overall.
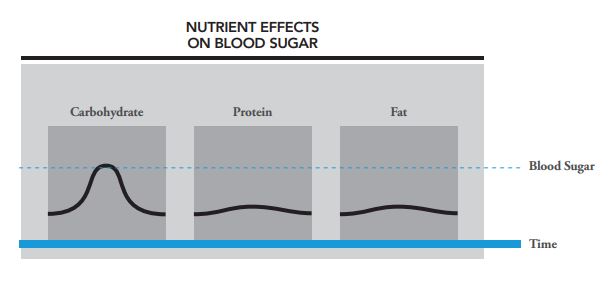
Having CFRD means you need to learn about how eating different foods will impact your BGLs. Carbohydrates are broken down into sugar in the body and therefore have the biggest impact on BGLs. Foods that are made up mostly of protein and fat have much less of an effect on BGLs.
Managing CFRD (CF Foundation)
Carbohydrates
Carbohydrates are the best energy source for your body. When digested in the gut they breakdown into glucose which is absorbed in the blood stream and transported around the body to be used as energy in muscles, the brain and all other organs. Carbohydrate foods include breads, cereals, rice, pasta, noodles, fruit, starchy vegetables, most dairy products and processed foods such as cakes, biscuits, soft drink and takeaway.
Carbohydrates produce glucose energy at different rates; some fast, some slow. The Glycaemic Index (GI) indicates how a carbohydrate food affects BGLs. The lower the GI, the slower the rise in BGLs will be when the food is eaten, resulting in sustained energy. It is recommended to focus on eating mostly low and intermediate GI foods for optimal BGL control. However, the inclusion of some high GI foods is usually still required to maintain overall calorie intake.
GI ratings:

Low GI foods include:
- Legumes such as beans, chickpeas and lentils
- Sweet potato
- Dairy products
- Fresh, tinned and frozen fruit
- Wholegrain breads, cereals, rice, noodle and pasta products
Your dietitian or CFRD educator will also be able to help you learn how to carbohydrate count and manage CFRD.
Fats
People with type 1 or type 2 diabetes are often advised to eat a low-fat diet to help prevent other health issues such as obesity and heart disease. This advice does not usually apply to people with CFRD. Most people with CF will be advised to continue to eat a high fat diet, however with the advice to select more of the good fats, such as monounsaturated and polyunsaturated fats.
Your CF dietitian will be able to prescribe overall fat requirements based on your age, BMI and overall health.
Protein
Eating protein alone does not have a big impact on BGLs, however when paired with a source of carbohydrate it can help to slow down BGL rise. Including a source of protein with most meals in important for overall health.
Alcohol
If you plan to drink alcohol, you should be aware of the effect it has on your BGLs. When you are drinking, your liver is busy breaking down the alcohol so it will release less glucose into the blood. This puts you at risk for low BGLs. Signs of being drunk are a lot like signs of low BGLs. If alcohol has clouded your thinking, you may not treat your low BGLs the right way. Those around you may not know that you have low BGLs and this puts you in grave danger.
If you are going to drink:
- Talk to your doctor or diabetes educator about how alcohol may affect you and how to best manage your CFRD.
- Only drink alcohol when BGLs are well-controlled.
- Do not drink on an empty stomach and continue to eat carbohydrate snacks while drinking g. chips.
- Check your BGLs after drinking to learn your response to alcohol (you may also need to check your BGLs during the night, especially if you drank too much or you have been physically active while drinking).
- Have a bedtime snack after drinking to prevent a hypo.
- Never drink alone; be sure to tell your friends that you have diabetes when you drink alcohol.
- Carry identification that states you have diabetes (diabetes ID bracelet or necklace).
- Be aware that alcohol may impair your awareness of hypos.
- Do not count the carbohydrates in alcohol towards your insulin dose.
Exercise
Routine exercise can help control your BGLs by making your body respond better to insulin. Be mindful that your body will use up more carbohydrate stores with exercise and you will need to monitor your BGLs during exercise.
People with CFRD can work out safely however should be aware of the following:
- Check your BGLs before, during and after your workout so you can watch your blood sugar patterns.
- Carry a source of carbohydrates with you e.g. glucose tablets.
- You may need an extra 15 to 30 grams or more of carbohydrates for each hour of intense or lengthy exercise.
- The blood-sugar-lowering effect of a workout can last as long as 12 to 24 hours, so you may need to eat an extra bedtime snack with carbohydrates on the days you’ve exercised really hard.
Reflux
Gastroesophageal reflux disease, more commonly known as reflux, is the backward and abnormal flow of the stomach contents into the oesophagus. Symptoms include a burning sensation in the chest or abdominal pain, sour taste, regurgitation of food or liquid, and chronic cough. Reflux is experienced by ~20-85% of the CF population, greater than those individuals without CF. Untreated, reflux can also cause pain or difficulty swallowing, damage to the oesophagus and oesophageal narrowing.
You may find certain foods trigger your symptoms. Discovering which foods make your symptoms worse can help you manage your reflux. Triggers are different for everyone. Common foods which may aggravate reflux symptoms in those with CF and the general population.
Common triggers:
- Spicy or fatty foods
- Caffeine
- Chocolate
- Citrus and carbonated beverages
- Peppermint/chewing gum
- Fermented drinks and alcohol
In order to figure out your triggers, it may be helpful to keep a food and symptom diary for a period of time. General dietary and lifestyle recommendations for the general population may also be helpful in managing reflux.
Tips for managing reflux:
- Small, frequent meals
- Physiotherapy prior to meals + large snacks
- Avoid lying down post meal/snack for ~30-60 minutes
- Avoid high fat meals 2-3 hours before going to sleep
- If overweight- aim for gradual weight loss
Avoiding alcohol, carbonated drinks and spicy foods before airway clearance may be useful in avoiding episodes during airway clearance.
Bone Disease
Bone mineral density (BMD) is a measure of minerals the bones contain, indicating how strong the bones are. People with CF often have a very low BMD, which may result in conditions known as osteoporosis and osteopaenia. This means that the bones are much more fragile and likely to result in broken bones, bone pain and changes in the way bones are shaped.
In CF, malabsorption of vitamin D and K, low mineral levels (e.g. calcium), and poor nutrition, can impair bone formation. Inactivity, low body weight, delayed puberty and chronic lung disease can all lead to weak bones. Diabetes, alcohol and smoking may result in a more rapid development of osteoporosis. The use of steroid medication pre and post lung transplant, in addition to immunosuppressive medications, can also increase bone loss.
To reduce your risk of CF related bone disease:
- Eat a healthy, varied diet and maintain a healthy weight.
- Regular weight bearing exercise to strengthen bones, as advised by specialist CF physiotherapist.
- Get at least 1 hour of sunlight daily to help your body make vitamin D.
- Have your vitamin D and calcium levels checked yearly, taking supplementation as required.
- Ensure you are taking the correct amount of pancreatic enzymes consistently.
- Have regular DEXA scans to screen for low BMD.
- Reduce intake of alcohol and avoid smoking.
Calcium
Calcium has an important role in the development of our bones, and keeping them strong. The best way to get calcium is from food. It is recommended that individuals with CF meet the Recommended Daily Intake (RDI) of calcium as per the general Australian population.
Recommended Daily Intake of Calcium

Information from Nutrition Guidelines for Cystic Fibrosis in Australia and New Zealand (2017)
Dairy foods are rich dietary sources of calcium: (at least 300mg/serve).
- 250mL (1x cup) calcium fortified milk (~400mg/serve)
- 250ml (1x cup) full cream/HiLo/Skim milk
- 250ml (1x cup) calcium fortified soy milk
- 200g tub natural yoghurt
- 100g tin salmon with bones or sardines
- 2x slices (40g) hard cheese
- 250ml (1x cup) custard
Calcium can also be found in non-dairy foods, such as:
- Meat, eggs, fish and tofu
- Beans e.g. chickpeas, soy beans and baked beans
- Green leafy vegetables
- Dried figs and apricots
- Nuts and seeds e.g. brazil nuts, almonds and tahini
Vitamin D
Vitamin D helps our bodies absorb calcium, therefore it is another important factor in bone development. The main source of vitamin D for most Australians is skin exposure to ultraviolet B radiation from the sun, although it is also present in small amounts in some foods. Foods which contain small amounts of vitamin D include; fatty fish (mackerel, herring,sardines, tuna and salmon), liver, eggs, fortified margarine and milk products. Vitamin D is included in CF-specific fat soluble multivitamin VitABDECK, although you may also need additional vitamin D supplementation (cholecalciferol tablets) if your levels are low.
Vitamin K
Vitamin K also has an important role in bone density. Vitamin K can be found naturally in some foods such as leafy greens and in VitABDECK.