Individuals with CF have greater nutritional needs, in particular energy (or calories), compared to the general populations. This is due to the high amount of energy the body uses to breathe, cough, fight infection in the lungs and poor fat digestion. The current guidelines estimate that the energy needs for individuals with CF are 110-200% higher than the general population, however an individual approach must be considered.
To meet these increased nutritional needs, individuals with CF are generally recommended to eat a diet high in energy (or calories). It is important to be guided by your CF dietitian as there is not a ‘one-size-fits-all’ method for determining energy needs.
It is important to follow a balanced diet including all food groups (unless otherwise advised) such as grains and cereals, fruits and vegetables, dairy products and protein foods like meat, chicken, fish, legumes, nuts and eggs.
Fat
Following a diet high in fat, can help to achieve the higher energy (or calorie) needs in people with CF. In general, adults with CF should aim for ~100g of fat per day. This recommendation may change if overweight or at risk of obesity.
The source and quality of fat is important. As people with CF are now living longer, the long-term effects of a high fat diet need to be considered, particularly for those with a higher body mass index (BMI). Following a diet high in saturated fat, can lead to negative effects on cardiovascular (heart) health. For some, increased intake of ‘healthier’ fats rather than ‘bad’ fats may be encouraged.
The four main types of fat are polyunsaturated, monounsaturated, saturated and trans fats. Trans fats can be grouped as saturated fats as they act similarly in the body. Polyunsaturated and monounsaturated are the healthiest forms of fats because of their positive health benefits.

Whilst saturated (and trans) fats are considered the least nutritionally beneficial source of fat, they may still be an effective option for those requiring a high energy diet to achieve or maintain a healthy weight.
There are many ways to incorporate more of the ‘healthy’ or unsaturated fats in your diet. Here are some ideas:

Protein
Protein is an important dietary component for those with CF, which is the same as general population guidelines. Many people with CF experience reduced muscle mass due to digestion issues with protein absorption. Proteins are the building blocks of muscles, therefore increasing protein, and exercising, can help preserve and build muscle mass.
Your CF care team can perform several body composition tests to determine your muscles mass. You can ask about this at clinic.
The quality of protein is important in CF, and people should aim for high quality dietary sources, such as those listed below.

Carbohydrate
Carbohydrates are a good source of energy and should be included in a balanced diet for those with CF and the general population.
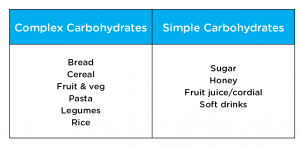
Complex carbohydrates are better sources of carbohydrates than simple carbohydrates. Simple carbohydrates are used up more quickly by the body and contain less nutrients for good health than complex carbohydrates.
Many carbohydrate sources also contain fibre, which is known to have an important role in bowel and digestive health, reducing cholesterol and stabilising blood sugars in the general population. See Bowel Health for additional information.
Salt
Individuals with CF lose three to five times more salt through their sweat compared to the general population. It is essential that salt (also known as sodium chloride) be replaced daily in individuals with CF, to prevent deficiency and dehydration. Signs and symptoms of salt deficiency and dehydration may include nausea, vomiting, muscle cramps, fatigue, salt crystals on the skin, dark colour urine, constipation and poor growth.
The amount of daily salt replacement needed is different for everyone due to varying sweat sodium losses between individuals. Sodium sweat losses can also be affected by illness, levels of exercise, dietary intake, hydration and the climate you live in. Therefore, salt supplementation should be reviewed on a regular basis.
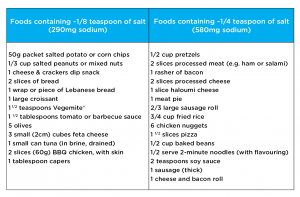
The recommended daily sodium intake for adults with CF is approximately 6,000mg per day or two to three teaspoons of salt (one tsp salt= 2,300mg sodium). The easiest way to achieve this is through adding salt to your diet.
Tips to increase salt intake and avoid dehydration include:
- Add table salt to food
- Eat ‘salty’ foods (see below)
- Always carry a water bottle
- Take salt tablets (e.g. Toppin)
- Drink commercial sports drinks (e.g. Powerade, Staminade, Gatorade)
- Drink commercial rehydration solutions (e.g. Hydralyte, Glucolyte, Gastrolyte)
Information from Nutrition Guidelines for Cystic Fibrosis in Australia and New Zealand (2017)
Fluids
Water
Every cell in the body needs water to work properly. You can get most of the water you need from what you drink, but you can also get water from many foods. The amount of fluid you need depends on your age, weight, activity level, general health and the climate.
As mentioned above, people with CF lose more salt through sweat and therefore require greater amounts of fluid to avoid dehydration. In addition, the thirst sensation may not turn on as quickly in individuals with CF, as for other people, or may not be triggered at all. Therefore, it is important people with CF do not wait until they feel thirsty to drink water. By the time the brain signals you to drink, you may already be dehydrated. Your CF dietitian can help you figure out how much fluid you need each day and help you decide on the best sources.
Alcohol
Advice regarding alcohol should follow the Australian Dietary Guidelines. The current recommendations advise that for health adults, intakes should not exceed more than 10 standard drinks a week and no more than four standard drinks on any one day. The less alcohol consumed, the lower the risk of harm from alcohol-related disease or injury. For some adults with CF, avoidance of alcohol is advised. This may include those with liver disease, pancreatitis and those taking medication where alcohol interacts or is not advised to be had in conjunction. People with CF-related diabetes need to be aware of the risks of hypoglycaemia with alcohol use.
The amount of alcohol to allow in your diet should be a decision made between yourself and your CF care team.