Most babies will start solids by six months when they are showing signs of readiness. Solids are given to supplement the milk intake and shouldn’t reduce the amount of milk taken. Breastmilk or formula is still the most important source of protein and energy at this stage. From nine months start to give solids first, then breast milk/formula. This allows for the natural transition from breast milk/formula to solids as the main source of nutrition intake by 12 months.
Signs of Readiness
Signs that your baby might be ready to start solids:
- Good head and neck control and can sit upright with little or no support
- Being able to munch and swallow and not automatically push solids out of the mouth
- Shows an interest in food – for example, they look at what’s on your plate
- Reaches out for your food
- Opens their mouth when you offer them food on a spoon.
Some behaviours that show lack of interest:
- Swatting at the spoon
- Turning head away from food
- Tightening lips when the spoon comes near the mouth
- Spitting out food that enters mouth
- Crying
Enzymes
If your baby is pancreatic insufficient, they will require enzymes (Creon) with any food containing fat, carbohydrate or protein. The only foods that can be digested without enzymes are fruits and most vegetables, all other foods (meat, fish, egg, nut paste, dairy, tofu and avocado) will need enzymes.
It is best to give the enzymes at the start of the meal to ensure the fats are digested and absorbed effectively. Remember, enzymes are only effective for about 30 minutes.
To work out how many scoops of Creon to give your baby, the amount of fat in the food needs to be calculated. One scoop of Creon covers, on average, four grams of fat. There are some excellent apps for fat counting, such as ‘Easy Diet Diary’ or ‘Calorie King’ to assist you. You can also talk to your dietitian about reading labels to measure the fat content in food products or recipes. They will go over examples with you to ensure you are confident in matching the Creon to your baby’s food intake.
Starting Solids
Starting a baby with CF on solids is the same as for any other baby, except for the addition of enzymes (if required).
Stage 1: Early introduction to food (4-6 months)
- Identify your baby’s readiness for solids: Are they avidly watching others eating, mouthing objects, still hungry after milk feeds, waking at night after sleeping through?
- Is your baby physically ready for solids: Can they sit independently, hold their head upright, able to swallow food, coordinating hands, eyes and mouth?
- Make it play-based: Allow your baby to play with and discover foods. This stage is all about first-tastes, so focus more on enjoying this time of discovery with your baby rather than the end goal of eating (that’s what milk is still for).
- Exploratory: Allow your baby to explore and learn to live with food. Exploring textures and foods with their hands. Most won’t go in their mouth! And that’s OK! This can be a messy time, however hands on fun fuels development. Try to dismiss the stress related to mess as a baby can sense your stress and may start to develop negative behaviours around food and mess.
- Create a positive experience: This is the start of your child’s relationship with food and creates the foundations for a life with food.
- Milk is still number 1: Solids are just a supplement to your baby’s milk feeds; so always give milk first. Food in stage 1 is seen as the tool to introduce your baby to new textures, tastes and sensory experiences related to eating and food.
When introducing the nine main allergens, ensure to do so one at a time and earlier in the day so you can monitor for any allergic reactions. Be aware that your baby’s poo will change colour and texture as new foods are introduced. It is normal for babies to gag frequently as they learn how to eat solid foods. Some babies can gag on purpose when they don’t want to eat something, which can last into their toddler years. It is recommended to speak to a health care professional if your baby gags, coughs or splutters regularly when being fed.
Stage 2: More Textures & Tastes (7-9 months)
- More structured mealtimes – Start to bring your child into the family meal times. Role modelling and connection are important to teach good habits.
- Milk is still the most important – Food is still seen as exploratory and an addition to the nutrition provided by the regular milk feeds. But perhaps offer solids at two meals a day now. Introducing thicker/lumpier foods and flavour combos as your child tolerates.
- Communication – Keep communication positive and light. Start to narrate and verbalise to your child what is happening and what is coming up so they start to understand routines and what’s expected.
- Self-feeding vs assisted feeding – Finger foods give your child independence and more sensory experience. Offering your child their own spoon to hold also develops fine motor skills and a sense of independence. Be accepting of mess and keep stress to a minimum. Messy play is multi-sensory and super important for your little one.
- New foods – Introduce new tastes and textures as much as possible and start to blend flavours. It’s good to begin to identify what foods your baby is very happy eating as these can be used as “safe foods” when introducing other new foods throughout this journey.
- Hunger and fullness cues – learn your child’s cues, especially fullness cues, such as crying, turning away, keeping mouth shut, shaking head, spitting out. It’s good to teach a sign for “all done” so you and your child can communicate with a hand signal. This assures your child that they have some say and can be understood.
From 7 months
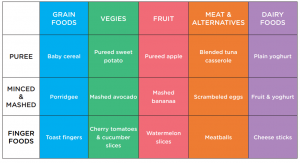
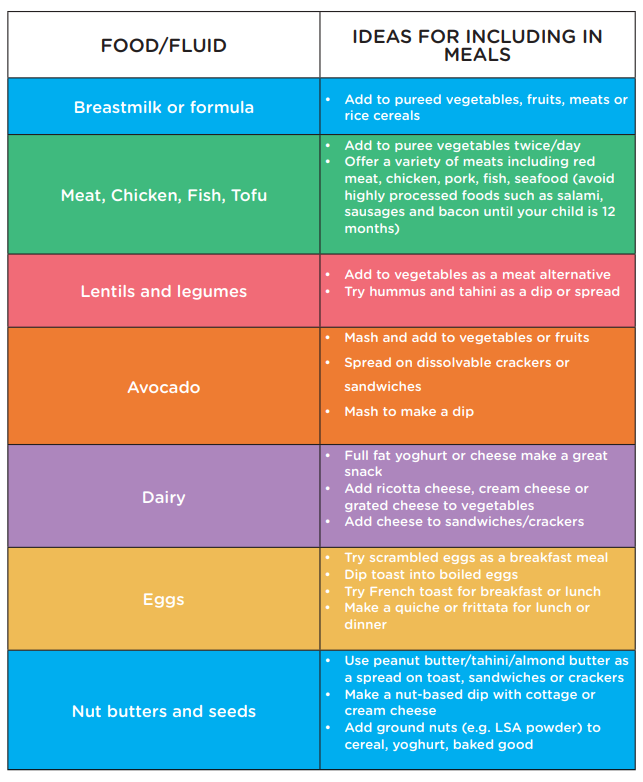
Begin introducing foods from all of the different food groups; grains (cereal), vegetables, fruit, meat and meat alternatives and dairy foods. Iron rich foods such as rice cereal (mixed with breast milk or formula), meat, fish, egg, tofu, lentils and legumes are good foods to introduce early. Iron rich foods are important for brain development and growth. You can also start to introduce protein rich foods such as yoghurt, custards and nut butters.
By this age the texture of the food can be a little lumpier than puree, however it does depend on your baby and how he or she copes with the texture. Mashed vegetables, porridge and eggs are good options for slightly chunkier meals.
From 8 months
This is a great time to introduce finger foods, which your baby can hold themselves and chew. Try finger foods such as toast, rusks, pieces of cooked vegetables (e.g. carrot, broccoli and asparagus), fruits (e.g. banana, watermelon, rockmelon and strawberries), milk arrowroot biscuits and strips of cooked chicken, fish or meat. This may be a messy time, however encouraging self-feeding is an important milestone for your baby to achieve.
Full fat dairy products are great, and protein is also very important for the growth and development of your baby. Nut pastes are ok to give to your baby on toast and bread (if your baby doesn’t have nut allergies) but avoid giving your baby whole nuts until they are three years of age.
From 9 months
Your baby can start eating some of the same foods as the rest of the family, as well as continued breastmilk or formula. Experiment more with finger foods and self-feeding. Soft fruits can be given in pieces, with skin and seeds removed and other types of food can be given in pieces or chopped. Changes in the texture of food is very important for your baby’s jaw and speech development.
Stage 3: 10+ months
- Starting to introduce balanced meals – Transition away from milk. Start to introduce firmer, crunchier foods as well as the softer foods already offered. Varied meals now become the main nourishment for your child by around 12mths+. By 10 months you can feed your baby three meals a day plus two to three snacks. Your baby can have high energy and protein rich foods and will still require about three to five milk feeds a day. If they require extra calories or high energy food additions, you will be guided by their CF dietitian.
- Make mealtimes sociable – Try eating with the family where possible. This allows for communication, role modeling behaviours and positive experiences. Kids learn by observing and doing within the family unit.
- Consider the environment your child eats in, minimise noise/distractions, try not to use screens/ipads/TV to occupy your child whilst eating, ensure the highchair/meal area is seen as a happy positive place (not a battle ground or punishment).
- Timings and routine – Kids thrive when there is predictability, consistency and routine.
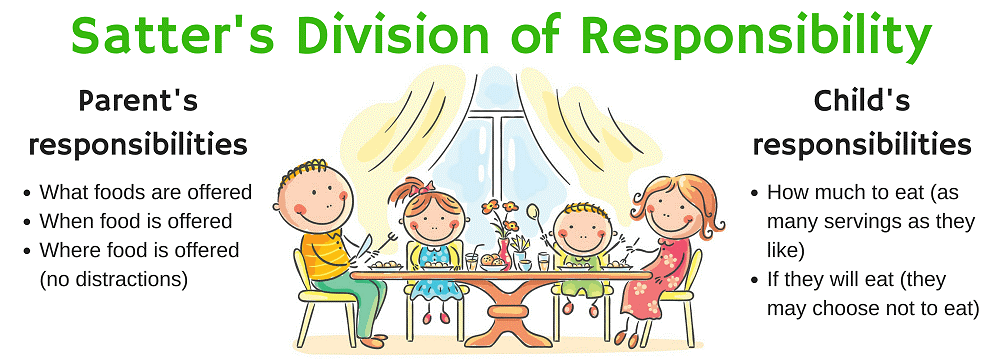
- Hunger and fullness cues – It’s useful to remember: “parents provide/children decide” and to never force your child to eat
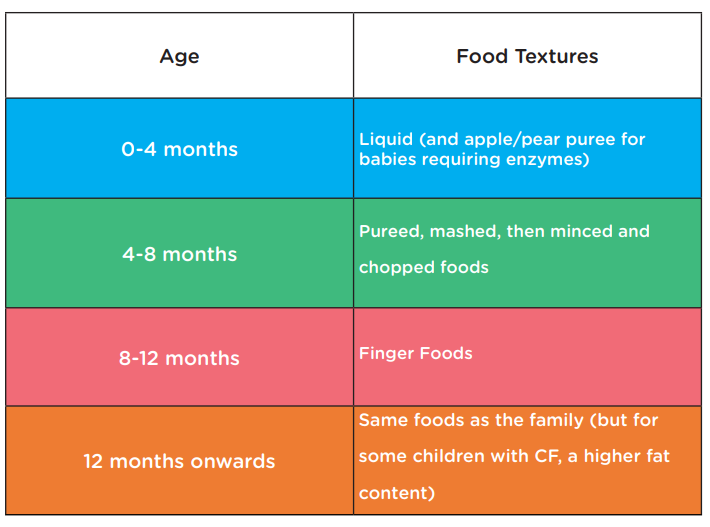
Below are some examples of the types of foods from each food group that fall into the different texture categories. If you would like more information regarding the introduction of solids foods, please contact your CF dietitian, child health nurse or GP. This is not intended for use as a meal plan.
Food Preparation
When your baby first starts having solids, it can help to be prepared and make up small batches of meals. Try and spend some time cooking up the different food items, freezing them into ice cube trays then placing in plastic zip lock bags when frozen. Calculate the enzyme dose required for each meal and write it on the zip lock bag. This allows you to have lots of different meal options on hand and know how much enzymes they will need with each meal. You can also write down the enzymes for each meal on your meal plan. Check out the sample meal plan in the ‘Charts’ section (Insert link).
High Calorie Meal Ideas
Infants with CF may need extra help to gain weight and grow well. This is due to their higher energy needs. Choosing foods naturally high in protein and healthy, unsaturated fats will assist with your child’s growth and development.
Here are some tips for including a wide variety of foods with high protein and healthy fats:
From Dietitian/ Nutritionists from the Nutrition Education Materials Online.